Intracerebral Hemorrhage Outcome Prediction
Introduction:Intracerebral hemorrhage (ICH) is the subtype of stroke with the highest disability rate among survivors. ICH has a 40-50% 30-day mortality rate, double that of ischemic stroke1, and 78% of survivors are disabled after ICH. The prediction of recovery after ICH remains a challenge, because ICH induced injury is highly complex. Clinical factors indicative of poor recovery after ICH include age, initial Glasgow coma scale, blood pressure, fevers, coagulopathy, and hyperglycemia. On the other hand, imaging features derived from both brain imaging data (e.g., MRI and CT) can also be helpful to predict ICH outcome such as hematoma location, volume ,and expansion, spot and swirl signs, and presence of intraventricular hemorrhage. Current predictors, such as ICH scores, rely on major cutoffs of ICH volume, presence of IVH, age, and location. Yet, small hemorrhages may have devastating effects on recovery, which is difficult to characterize. There is a critical need for accurate prognostic tools that can combine multiple clinical and imaging factors to identify patients at risk for poor outcome.
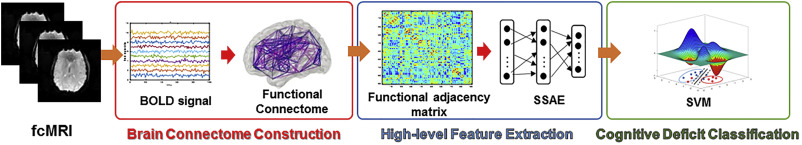
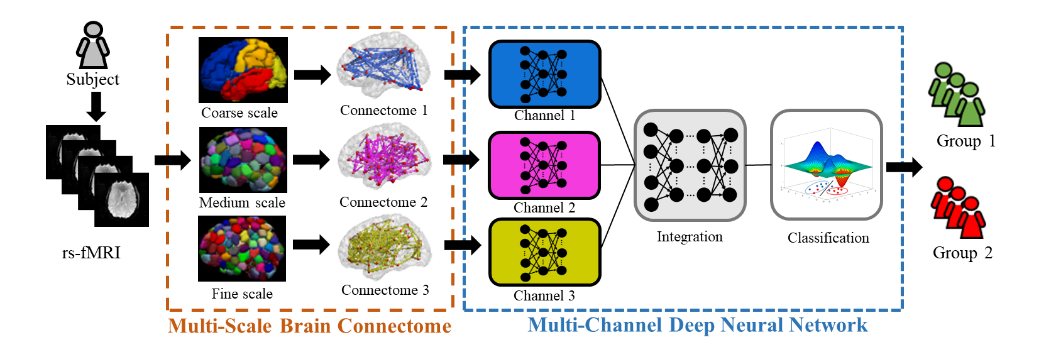
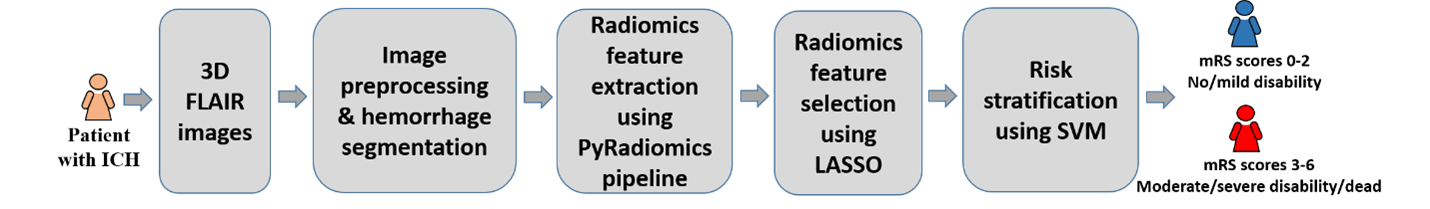
We have demonstrated that traditional machine learning model using radiomics features derived from T2-weighted FLAIR images can identify ICH patients likely to have unfavorable outcomes. We have built an SVM in a supervised fashion from a cohort (patients with ICH who have 3-month outcomes) with a set of prognostic radiomics features. The constructed model is able to evaluate whether a new patient belongs to no/mild disability (modified Rankin Scale (mRS) 0-2) or moderate/severe disability group (mRS 3-6).
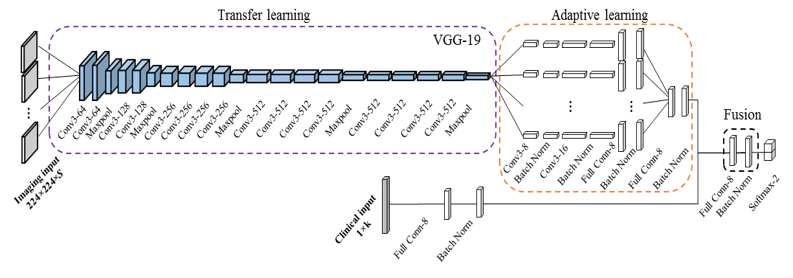
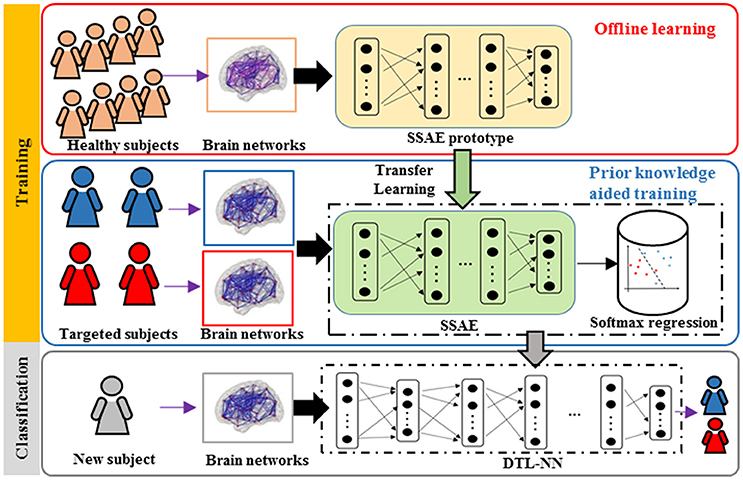
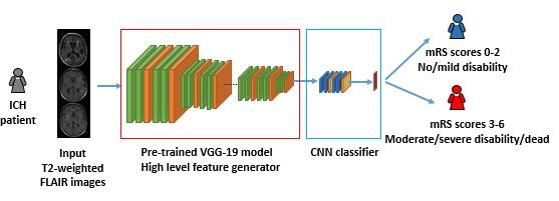
Though the results of our SVM model are promising, we have also demonstrated a superior performance of deep learning models on the fusion of clinical and FLAIR imaging data to identify patients with ICH likely to have unfavorable outcome. [He, et al., 2019] To mitigate concerns regarding insufficient data for training a deep learning model, transfer learning and data augmentation techniques were employed. We employed a pre-trained VGGNet-19 model as a feature generator to learn high-level features from input FLAIR images. Such a prognostic model can potentially help with the treatment decision and rehabilitation strategy optimization. Our study is hypothesis generating and a larger multidimensional study is required to validate our approach.
Reference:
He L., Chen M., Li H., Wang J., Khandwala V., Woo D., Vagal A., Deep Learning Model to Predict Patient Outcome in ICH using Fluid-Attenuated Inversion Recovery Imaging Data. Radiological Society of North America, 2019, Chicago.